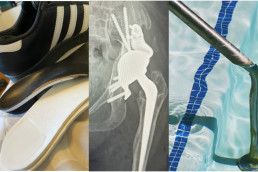
The specialist therapy jigsaw for hip rehab: physio, hydro, podiatry
It’s now 9 weeks since my complex hip revision surgery. In the last few weeks I’ve seen various therapists who each deal with a different part of the rehab puzzle: Physiotherapy, Hydrotherapy, Podiatry and Chiropody. With a lifetime of hip dysplasia, bringing this together requires a slow and steady approach that’s a lot more tortoise than hare….
Physiotherapy
I’ve been seeing a physio every 2-3 weeks since my surgery, and physio is definitely the centre of my recovery plan. Whilst the surgeon sets the guardrails around my rehab (the pace and limits to protect the hip whilst it stabilises) it’s my physio who I see as the key person guiding my progression. More recently my exercises have been about getting specific muscles to engage that will restore particular day to day movements; sit to stand, sliding and lifting my leg independently, stepping up and down, bending my hip fully to 90 degrees in some positions. And walking reciprocally with my crutches (mimicking a more natural way of walking and taking more weight through my operated leg).
I found this physiotherapist over 15 years ago and her knowledge of how different my ‘baseline’ is to a normal set of hips and knees has been critical. She also gives me advice for hydro and podiatry and I let them all share my personal data/liaise if they want to.
Hydrotherapy
After my last post-op consultation I was allowed to start hydrotherapy. This is both a relief (I’m a swimmer and I’m really missing the water) and extremely tiring. My first session was overwhelming, both physically and mentally as I was so anxious not to do ‘too much’. I had my second session yesterday, which was much better because I knew I’d been OK after the first one. But still tiring - I slept so well last night and I’m sore today. I always progress faster once I start hydrotherapy because the support from the water (and so being 50% not 100% weight bearing) means I can make more movements for longer - stand/sit, walking, cycling movement, leg raises etc. We are being a little cautious about some movements like abduction, and not adding resistance like flippers yet. But I can do so many more repetitions of my exercises in the water. Plus I get a proper shower at the end, which still feels like a luxury until I’m allowed to step into a bath to take a shower at home.
Podiatry (orthotics)
I first started with orthotics a few years after my initial hip replacement. My knees, ankles and feet are all part of my unusual biomechanics - none of them are ‘normal’ and there’s a lot of hypermobiity (ie they’re loose, so add additional instability to way I walk). Post my hip replacement, I got some custom orthotics for the first time in both my shoes - to help correct a small (1cm) leg length discrepancy, and to help stabilise the position of my knees and feet when I walk. After my right knee replacement, the leg length discrepancy became more acute (more like 2.5cm) and so for the last 3 years I’ve had an outer shoe raise as well as inner orthotics. It’s amazing what can be done by a good practitioner (gone are the days of the big black surgical boot).
After my recent hip revision surgery, my new metal hip socket is a bit bigger and less worn, so I’m back to around 1cm difference again. It will take about one year of continuous improvement before we know exacely where it will end up - so I don’t yet want to spend money on a new permanent solution (custom orthotics aren’t cheap).
So, last week I saw the podiatrist (who I’ve also been working with for a number of years) for an interim solution. A couple of ‘shims’ to about 8mm (think thick bits of insole custom cut to size) under my most recent inner left orthotic, has allowed me to remove the outer shoe raise. I’ve only had this solution for three days yet I can already feel the difference - the position of my left knee and ankle when I walk is much straighter and more stable. This will become really important when we get to walking without crutches, and right now, it helps with physio exercises like sit to stand from a chair, because my knee can take more weight. My hip muscles are a little sore as they adapt to a slightly different (correct) use of the muscles, which have all been traumatised by the surgery.
Chiropody
Not an obvious essential therapy, but when you’ve had any hip surgery, by far the hardest thing for a very long time, is reaching your feet! Putting on shoes and socks needs assistance, and cutting your toe nails is just impossible. Comfortable and healthy feet are essential when you’re re-learning to walk. So my trip to the local chiropodist this week felt like a birthday treat!
Putting the puzzle together, more tortoise than hare
Major and complex hip surgery - something I’ve had more than once in my life due to my hip dysplasia - takes a long time to fully recover from. In fact, physio and conscious monitoring of how I walk and move is just a way of life and constant progression.
A tortoise, not hare mindset is important! Slow and steady, piece by piece, rebuilding movement, range, strength and stamina is a very particular sequence, guided by experts. Two days after my op, having orthotics managing my knee position was not as important as just getting me mobile on crutches. 9 weeks on, if I want to progress further, it is important. Because my knee not my hip was beginning to limit what I could do.
Every time I have surgery I’m amazed by how it does come together, bit by bit, with the guidance of experts and me diligently doing what they ask every single day. Every time I’m impatient for quicker progress (not a naturally patient person!). I have to work hard to calm my ‘inner hare’ and keep the tortoise moving forward. Tortoise Pringle will win the race and it was never going to be a sprint!
Thanks for reading and supporting my progress. Love to you all x
Jill Pringle was born with hip dysplasia (CDH/DDH) in 1971. She had several hip and leg surgeries at Sheffield Children’s in the 70s and 80s, and as an adult has had a left total hip replacement, total knee replacement (opposite side) and most recently a full revision of her original hip replacement. She writes about her surgeries and has also undertaken various walking challenges, to raise awareness of hip dysplasia. You can listen to more of her story on the podcast here.
Before and after hip xray: hip replacement to hip revision
So here is my new hip! With a handy before (hip replacement) and after (hip revision) comparison Xray. First thing that strikes me is that there’s a lot more metal than pelvis now. Due to my hip dysplasia, I’ve never had much pelvis on that side (which was the difficulty with getting my childhood reduction surgeries to stick). The challenge for the hip revision was to extend the socket and so that bit you can see on the right hand side of the Xray is the custom 3D printed metal socket doing just that job.
I was talking to a friend a few weeks ago about the fact that I was finding it difficult to visualise my new hip because I hadn’t yet seen an Xray. And in that conversation it became clear how much I understand my condition through the hip Xrays I’ve had through my life. I have never not had a mental image of what my pelvis and hips look like and I suspect that’s the same for anyone diagnosed with CDH at birth. And so I suddenly felt lost. Now, I ‘get it’. I can see what my orthopaedic surgeon has done and I can finally connect the image with how it feels. It’s reassuring to me.
The last few weeks have been very boring. I’ve been diligent and consistent with my physio exercises, and maintaining all the restrictions around precaution height and restricted movements. For the last 3 weeks I have at least been able to go for longer walks on my crutches, but I still can’t go anywhere where I need to sit.
I saw my Xray when I had my 6 weeks post-op check up this week with my orthopaedic consultant. He seemed pleased with my progress - wound is healed well, no infections, no thrombosis, nerves appear to be undamaged and the leg is “pointing in the right direction”. He was also happy that I’m taking things slow and steady - something he wants me to continue for the next 7 weeks. I am still to stay on crutches as by far the biggest risk is falling. As he said, in essence it’s like having a big fracture in my pelvis and that needs caution. I guess if I fall and damage this, there’s no more pelvis to play with, and now I’ve seen the Xray my brain gets that so much more.
So it’s more of mostly the same.
- I asked if I can swim yet, we compromised on me adding supervised hydrotherapy into the mix, as long as I take it carefully.
- Continue with the physio with the advice of take it slowly and carefully.
- I can however start to play with lowering the precaution height of chairs very gradually - eg removing one of the three cushion - as long as I never bend more than 90 degrees. As this progresses it will give me a little more freedom to at least walk further if I can sit on a bench or in a cafe to rest half way.
- Still no bending, twisting or climbing into the over-bath shower though….so still the strip wash regime continues into September. At least when I go for hydrotherapy I’ll be able to have a shower afterwards - can’t decide if I’m more excited about getting in the pool or having the shower!!
If I'm honest, I had mixed feelings after my appointment. Obviously the overriding positive feeling is that I’m progressing well in his expert eyes, and that surgically he is considering this a success. But I also had a feeling of dashed hopes. Hopes that I could start to do more, more quickly - particularly swimming or driving, which would give me more independence.
But this is not my first surgery and I know that by sticking to what I’m asked to do, the end result will be more positive. This too shall pass. And my independence day will come :-)
Meanwhile, stay tuned, thanks for following. Love to you all x
Jill Pringle was born with hip dysplasia in 1971, in Sheffield (then called congenital dysplasia of the hips). She's had many orthopaedic surgeries as a child and adult. Jill writes this blog to share her challenges with walking as a differently-abled person.
Hip Revision Surgery: my first day and night in hospital
I had my total hip revision surgery just over 1 week ago. It’s been a full-on week or so, as I start to recover from a major surgery.
This is not my first hip surgery. Born with bilateral hip dysplasia (DDH) in 1971, orthopaedic surgery has been a regular cadence throughout my life. As I child, I had several surgeries to finally get me walking by the age of 3 and a half, a femoral plate removed when I was 7, a leg lengthening surgery aged 16, a total hip replacement (THR) aged 32, a knee replacement at 50 and now this revision on my original THR.
I had my surgery at the elective orthopaedic centre (SWLEOC) at Epsom Hospital in June 2025.
The morning of surgery
I had to be at hospital for 7am and I’d been fasting since the night before. I had a big glass of water at 6am then nothing. I showered in the same special wash I’d been using for the last 3 days. Despite my hunger, the journey was calm and uneventful as my partner drove me there. Heading for major surgery is a weird feeling, not unfamiliar to me. I know it’s what I need, and have been waiting for it, yet it’s scary. All the what ifs and risks are bubbling under the surface, and just that feeling that I’m about to put myself through intentional pain and trauma is unnatural.
Along with 6 other patients, my partner and I were taken up to pre theatre. It was unexpected and reassuring he could come with me - my last surgery was just past covid so no visitors were allowed at all. It helped to have a friendly face there, someone who loves me. I gowned up, had the usual pre op checks to make sure I was fit enough, ensure no infections, scratches or bruises. They drew a big arrow on my leg and wrote LEFT on it for good measure!
The anaesthetist visited and explained it would be a spinal pain management with a sedative, rather than full general anaesthetic. For me this was good news - I have never reacted too well to the GA hangover. He inserted a cannula in my arm so they could take blood and to later administer the meds. He then listed all the side effects and risks, as they must for informed consent. And then something new happened. The room started spinning, I got dizzy and hot, and I fainted. Next I knew was my partner telling them I don’t like masks on my face, as I came round. It’s called a vasovagal response but to you and me, it’s fainting. It’s a common feature of my previous post-surgery journeys because my blood pressure is naturally low. But I’ve never done it pre-op before. First time for everything!
They put me back on the bed and I was quickly back to normal. The staff reassured me that it’s quite common and all good. My surgeon arrived, which was reassuring as he’s been my consultant since 2002. He explained the hip revision surgery again, showed me a diagram of the hip joint that’s been built, and said I was first up in theatre so not long to wait. It would be 4-5 hours and I might lose blood and need transfusions. He also reminded me it’s going to be a long recovery where I need to be slow and steady, not take any risks for the first six weeks, until the new hip sets in place. He confirmed I will be weight-bearing with crutches but need modified exercises due to the much higher risk of a revision dislocating and the need for the joint to set in place.
Before 9am I said goodbye to my partner, and was wheeled in a chair to theatre. The scene when I arrived was actually fascinating - like a scene from a movie, with lots of people in the background in blue hazmat style suits readying things! I recognised the anaesthetist team, who asked me to transfer to the operating table, undid my gown at the back, asked me to lay on my non operating side then hooked my cannula up to the drugs machine. “First anti sickness” says the anaesthetist. “OK now the sedative." I asked ‘should I be feeling sleepy?. He says yes. And that’s all I remember.
The afternoon - coming round in PACU
I think I remember them first bringing me round in theatre, I have an image of a few people in gowns/masks looking at me and saying hello, including the surgeon. The next thing I remember is being in PACU, with a two lovely smiley nurses, Pam and Suzy, telling me where I was and that they were looking after me. I was hooked up to fluids and they explained that I also had an arterial line on the other side so they can take bloods regularly to check my haemoglobin levels. They gave me my phone and I messaged my partner to say Hallo and sent a selfie, so he knew I was OK and could let my sister and colleagues know. This was at 2pm. The surgery had taken 4.5 hours.
Regular observations (obs) of my blood pressure, temperature, oxygen levels continued. I had some water, a cup of tea and some toast which was heaven. They asked me to wiggle my toes, see if I could lift my legs, and seemed happy. I had no pain, the epidural was still attached and would be all night. And then I almost, but didn’t fully faint, to add a bit of drama. Once again it was over quickly with some oxygen and a big fan (which has become a staple post-surgery friend for me).
The anaesthetist and my surgeon both visited me. They were un-fazed by my fainting - long surgery, lost some blood, I’m lightweight, and I’d been fasting.
My consultant orthopaedic surgeon explained that the surgery went to plan, so he was happy. He reminded me it remains very fragile in there - I have so little pelvis on that side in the first place to work with. And he reiterated no risks at all, slow and steady for 6 weeks, just focus on letting the bone and metal joint bond so it gets nice and secure. He reminded me only to walk with crutches, no twisting, carrying, crossing my legs or over rotating the hip, and be hyper-aware of my precaution height - the lowest furniture I’m allowed to sit on so I don’t end up bending to to 90 degrees or more. More on this in a future blog because, frankly, it’s quite limiting!!
My partner came to visit about 4pm. I heard him coming down the corridor, and it was the happiest thing to see his face and get a big kiss. It was lovely to chat, although I expect I made no sense whatsoever (nothing new there he’d say!!). He brought pics of Dudley, our cat, saying hello :-) I had sandwiches and a protein shake.
Obs continued throughout the evening, once my legs were better thawed they hooked pain meds into my epidural. Then I was sick so they gave me anti sickness injections and fluids. They had to keep spraying my legs, waist and trunk with an ice spray, to test what I could feel below and above my waist whilst the epidural was still in - to make sure that any spinal pain relief was not creeping up my body as that could impact my breathing. The regularity of my obs was a reassuring drumbeat.
The evening - a long night of intermittent sleep, pain, meds
As the evening progressed, many of the people who were in the waiting room with me that morning were mobilised up onto crutches and left either to go home, or down onto the ward. I remember this from my first hip replacement where as the youngest (but also the most complex) I had taken a few days to mobilise whilst all the 70+ patients were whizzing around on crutches on the same day!!
That first night I stayed in PACU. I had a new nurse called Andrew overnight who looked out for me and a couple of other patients all night. With regular obs, ice sprays, anti-sickness and other drugs, and the fan on all night to help keep my temperature stable. My legs slowly thawed - ironically it was the non-operated leg and ankle that was the last to regain all feeling some time the following day.
And just like that, hour by hour, me and my new hip made it into day 1 post op. I could not be more grateful for the care and good humour of all the staff at SWLEOC Epsom Hospital pre and post op that day. Friendly people, amazing professionals. Thank you all so much.
I made it through that first day. And now the post hip-revision journey begins.
More to follow in a few days…..thanks for reading the blog! Love to you all xx
Jill Pringle was born with bilateral hip dysplasia (DDH) in 1971. She writes this blog to share her experiences of walking and living with this common disability.
Time for a refit. Hip revision surgery and DDH
It’s 22 years since I had a total hip replacement, needed because I was born with hip dysplasia (DDH). Hip replacements of that time last about 15 years, so I feel lucky that I’ve had over 20 from mine. But over recent years, walking without sticks has become more difficult, and in December I learned it’s time for the hip revision surgery.
What is hip dysplasia?
Dysplasia means abnormality. In short, my hips didn’t form properly. When I was born, the socket was too shallow on one side, which means it doesn’t rotate properly. But on the other side, the socket and part of the pelvis were just missing. I spent my early years in and out of Sheffield Children’s Hospital, with open and closed reduction surgeries and in a hip spica between them. You can read more about that in some of my previous blog posts – from my early memories of surgery, to my leg lengthening, my hip replacement and a stabilising knee replacement in 2022. Like many people born with DDH, surgery is just part of my life.
Why does a hip replacement need revision?
Quite simply, the parts, and the fixings, start to wear. Just like a real hip. We humans take a lot of weight through our pelvis and hips, and they are made to move. Don’t know about you, but it’s quite for me to actually stand still. Should have been a jack-in-a-box!
The polyurethane lining in the socket starts to wear, just like with cartilage, and the tiny bits of plastic get into the bone tissue around the hip joint. This causes something called Lysis – which means the bone stops forming so well, and softens around the fixings. And so the socket starts to get looser and some of the parts need replacing.
I mean really, it’s a bit like a shelf. Nice and secure when you first put it up, 20 years later it’s come a bit loose and so needs taking down, some filler and new rawl plugs (if you’re lucky) or if not so lucky, you have to drill in slightly different places and plug the old holes. If anyone medical reads this I apologise for the massive oversimplification of your immense skill.
But it’s kinda what my hip revision surgery is going to be. So, the shaft into my femur is still secure, so my surgery will focus on replacing the ball, the socket and the polyurethane liner. And using bone filler to secure it in place and plug any holes.
A ‘3D printed’ bionic hip
Tech can be frustrating (someone changes the button you knew on Microsoft Teams LOL!). But it’s also amazing what it’s enabled in the medical field. So my new hip has essentially been ‘custom printed’ to fit my strange little pelvis perfectly. How amazing (again, if a little simplified). And how lucky to live in a country where I get to have that surgery.
Four days to go
So I’m now on the final prep journey, with 4 days to go until my hip revision surgery. I’ve had my pre op assessments, had the handover at work and I've been swimming as much as I can, and sorting out my home for what I’m told will be a “no picnic” kind of rehab. More on what’s involved in that, and some unusual places to get what I need, in my next post.
Until then, I’m hoping for as much sunshine as possible whilst I can still get out and about. Hope the weather is kind to you all too, wherever you are reading.
Until next time….
Jill Pringle was born with bilateral hip dysplasia in 1971. After an early childhood in a hip spica and various surgeries, she now writes about her experiences of living with her DDH, her surgeries and her walking challenges to raise money for Steps.
Mind the gap, find the gap! Trains, parking and the social model of disability.
In the last two weeks I have taken my first train journey and my first solo drive in the car, since my op. Such big steps forward in lots of ways. As it turns out they were very hard steps to take on crutches with poor balance.
I’m in this weird period right now where neither leg is the good, dependable one, and that’s a first for me. It’s really reminded how differently-abled I can be and what the social model of disability is getting at.
Mind the Gap – the train journey
I’ve had intermittent periods on crutches my whole life. I’m pretty mobile on them, relatively quick vs. a novice, and accustomed to using them on public transport. But my first trip into London by train since my knee replacement, was just horrible.
I remembered to take a train 30 minutes earlier than necessary, so I had time for lifts in connecting stations and take my time across a busy London concourse like Victoria. But getting on, and particularly off the train to change, was more difficult than I expected. Clapham Junction is an amazing feat of engineering and I’m always in awe of how many lives it connects every hour. But the platforms are curved, the train leans away from the track and the chasm that awaits when the doors open is huge in both height and width. Before my op I was handling this by taking weight on my right leg. Now it’s Hobson’s Choice which leg is the weaker. Kind people on the platform try to help, but essentially try and grab my arms (which stops the crutches doing their job and puts my weight on the legs I’m trying not to rely on).
I finally got off with a lurch and a hope. It hurt a bit but I was mostly relieved that I didn’t fall into either the gap or the crowd waiting to get on the train. It’s safe to say that by the time I got to where I was going I was quite traumatised really. And so spent most of my lovely first Choir rehearsal in London dreading the journey home.
Next week I’ll be trying this journey again. I will try to find staff at the station and the right door for the guard on the train, so I can warn them I may need assistance at Clapham. Which, of course, requires more time and planning.
There is nothing easily done about this; old Victorian platforms were not built with disability in mind and I’m not suggesting that Clapham has to be rebuilt, for me. I also know that for some people it’s much harder; they have to call ahead to pre-arrange travel to even get access, and I also know that others in the DDH community would love to walk as far as I can on crutches. We’re all different.
It was simply an eye-opener into travelling with a disability - that I’d forgotten. For a while, I suppose, I’d taken trains for granted.
Find the Gap – the car park
I can now drive about 40 minutes without pain in my right knee or hip flexor. Which means I no longer need my partner to arrange his day around any medical appointments. That’s great for both of us, it gives me independence and I’m grateful for it.
But I always experience the background anxiety of “where am I going to park?” I need to make sure I can get out of the car and then be even more certain I can get back in it when I return!
I am able to walk too far (even on crutches) to qualify for a blue badge. I certainly don’t usually need to be right next to the door of a shop (unless I’m carrying a shopping bag in which case it’s a shuffle, placing the bag down on the pavement every few yards).
The big car parking challenge for someone like me is finding a space at the end of a row, where I can open my car door either into a grass verge, a pavement or the road – so that I can get the door all the way out. I need this clearance to swing my legs out and round together (without full flexion in my knee) and then I need to use the door to lift myself up out of the seat. I can’t go in and out sideways one leg at a time. Once I can stand up I need to turn around, lean into the back seat or over to the passenger seat, get the crutches out, put them in my arms and then close the door. Let’s just say it takes a while. Most people are patient and wait. Most.
On the way into a car park, I do at least have the chance to control this - finding the most suitable space or if there are only narrow spaces left, leave. What might happen on the way out is always on my mind. I have mini. If I can’t find an end space then I have to leave enough space next to me to get out at the side. Someone with a big car or van invariably sees the next space as a great place to park - it gives them plenty of room. Why wouldn’t they? It makes perfect sense and they don’t know that I need that extra room. So I return to my car and can’t get open the door even a fraction. Pre-op, I would have gone in the other side and scutched across the seats and hand break as my knee, whilst painful, was hypermobile and very loose. Less of an option now where bending is more challenging the knee is more robust.
So the options are to contort and cause myself some pain and potentially put some things in my upper body out of alignment for a couple of hours; or if it’s too tight, wait for them to come back to their car. The only other alternative is to park in a disabled or parent and toddler space and hope I don’t get a fine. Hopefully I get the can just find an end space.
Again, I’m not alone in this, many older people without a lifelong disability have the same challenge. And I’m happy to be finally out and about. It’s just this is on my mind from the minute I consider the trip, weighing up do I go out to this thing and risk it, or not.
The social model of disability
My reason for sharing this is not to rant or ask for sympathy. I don’t resent others’ mobility and if you have it you should use it – I would! I have a pretty ‘it is what it is’ attitude borne from 50 years being a differently-abled walker with huge variation my mobility across different periods – sometimes highly disabled by the world around me, other times not much.
Since part of my motivation for creating this blog is to share what it’s like living and walking with just one limiting condition, I simply want to share my experience. And ask you to take just a moment to consider what you might take for granted.
If you want to learn more about the social model of disability, there’s a great 3 minute video on the Scope website here that explains it well.
Thanks for reading. Until the next journey…
Jill Pringle was born with bilateral hip dysplasia in 1971. She has had numerous surgeries as both a child and adult, including open reductions, leg lengthening, and both hip and knee replacements. She writes this blog and walks to raise money for Steps Charity – you can donate here.
3 months post-op: back to hip rehab to get off crutches
This week it’s three months since I had my knee replacement. Turns out that quite a lot of people born with hip-dysplasia develop knee problems due to the abnormal wear that comes from the way we walk. It’s been lovely to hear from these people who have commented on my @WalkingJill blog posts, and gave me a chance to hear what to expect after that initial and very painful first month.
So where am I at three months in?
- I’m very mobile locally, on my crutches, and back to walking my virtual Pennine Way – using my daily rehab walks to clock up 1-2 miles per day. Since 1st March I’ve managed 36 miles and there are 32 miles left to complete the challenge I had to abandon last year.
- I’m able to walk between the kitchen and lounge without crutches (albeit lobsided) and I can now stand for about 10 minutes unaided. I can make a cuppa or lunch and carry it to the lounge to eat or drink. Compared to a month ago this feels like a luxury!
- Doing certain physio exercises can be painful, and sometimes my knee aches after a long walk, but I’m not really in much pain.
- My knee isn’t swollen and I can see the shape of my lovely straight leg – the first time I’ve been able to say that in 50 years!
- I can sit at a table with my leg bent at 90 degrees for about an hour before I have to get up and move around to unlock it. This means I can sit at a desk to do a bit of work and can eat at a table.
- I’m back swimming in the fast lane in the local pool and I can get in and out via the ladders rather than using the chair hoist.
I’m not yet off crutches to walk any distance, nor am I driving or have I braved public transport. (Next time you’re getting on and off a train or tube take a moment to consider how you’d ‘mind the gap’ if you couldn’t stand on just one leg to step up and out easily, couldn’t hold on to any handles, and you’re surrounded by lots of people in a rush who are focused on their phones not where they’re going….)
It always comes back to the left hip!
My left hip has always been the weakest point in my body. That’s the one that wasn’t fully formed when I was born and has had so much surgery including a hip replacement 19 years ago. So it’s not really a surprise that getting me off crutches isn’t really about my new knee. It’s about getting my left quads and glutes strong enough to take more of the weight than before and retraining my brain to let it. It’s also about correcting the leg length discrepancy.
As well as physio exercises that now extend to both legs, the next big step is a podiatrist appointment to re-work my orthotics and potentially add a small raise to the sole of my left shoe. I used to have my left shoes adapted in that way but after my hip replacement my leg length discrepancy lessened and so I was able to have orthotics inside the shoes (my left foot is a whole size smaller than the right so there’s extra room in that shoe!). But now my right leg has been straightened there’s a good inch or so more discrepancy and no more room in the shoe! My first appointment is next week, and once I have some adapted shoes I should be stable enough to walk unaided.
Until then I’ll be whizzing around Walton using my crutches reciprocally, giving my triceps a work out as well as clocking up the miles!
Thanks to everyone who has been cheering me on xx
Jill Pringle was born with hip dysplasia and has had multiple surgeries including open and closed reductions, leg lengthening, hip and knee replacements. She walks and blogs to raise awareness of DDH and to raise money for Steps Charity.
Getting my new knee moving: hydrotherapy
Yesterday two really great things happened – I got into a pool and I slept.
You all know that I love to swim. Walking down the steps into the hydrotherapy pool yesterday almost made me cry with joy. As I walked deeper into the water my body relaxed limb by limb – the first time since my knee replacement two and a half weeks ago. I felt supported and the heat was like jumping into a radox bath. My 30 minute session with my physio went so quickly, but in that time I was able to squat a bit, paddle and bend my legs, stand on tiptoes and my heels, and walk without tensing my upper body. Some of the movements hurt a bit, yet the joy of moving far outweighed that. For the first time in nearly three weeks I felt like I had my body back.
This knee replacement is definitely the hardest of my surgeries. I was warned that for all people a knee replacement is harder to get over than a hip replacement. As you know from my last blog post, not sleeping has been a real issue. Not being able to bend the leg has limited the positions I can lay in and my body wakes me every hour or so to move. Whilst lying on my operated side can help me get to sleep, it’s painful for the knee and increasingly for my right hip. So, it’s a constant nodding and waking routine where I get limited rest in each 1 hour cycle – also apparently normal with knee surgery.
Then last night, after hydro, it was easier to turn, and instead of waking hourly with big gaps in between snoozes, I managed a couple of 3 hour sleeps. My joy today is palpable.
My scar has now just about healed. Just a couple of steri-strips and scabs to come off naturally over the next week. I also took my last blood thinner last night, so I’m looking forward to an evening in front of the TV tonight without the shivers. And by the end of next week I can finally lose the surgical stockings and go back on HRT, so hopefully goodbye to the hot flushes too.
My days continue in a rehab routine of threes. Physio exercises three times a day; Walking in my shoes/orthotics for 15 minutes three times a day; CPM machine for 30 minutes three times a day, and pain meds three times a day. I also now have to start varying how I sit every 30 minutes – legs up, legs as down as a I can get them. All day this has me like an “ill-sitting hen” as my mother would have said. My cat, who thinks my lap is her personal property on-call, is not at all amused by this constant moving.
But it’s all progress. Small steps towards a more normal life. I’m intrigued to see how I’ll walk in six months’ time. My right leg is now even longer than my left so I already know I will need even bigger orthotics in my left shoe. But that’s a job for eight weeks post-op, not three.
For now, the next step is to use more hydrotherapy and physio to get my knee to 90 degrees within two weeks, when I next see my consultant surgeon. He was very clear that if I can’t do that, he will have do a manipulation. He was also honest that “you really don’t want that” and that it will be extremely painful. So that’s a clear goal – 90 degrees under my own steam in two weeks. At the moment I can get 55 degrees on the CPM machine and 45 degrees myself. Which I guess is half way to target.....
I’m back in the hydrotherapy pool on Monday and I can’t wait. Until then, have a wonderful weekend. Jill xx
Jill Pringle was born with bilateral hip-dysplasia with her left hip dislocated. She has had multiple corrective surgeries including leg-lengthening, a total hip replacement in 2003 and now a knee replacement in 2022. Jill writes this blog to raise awareness of hip dysplasia and walks to raise money for Steps Charity Worldwide.
Sleepless in Surrey: my knee replacement
I had my total knee replacement 10 days ago, just 2 weeks after my 50th Birthday. By my counting this is my 12th orthopaedic surgery, my last being a total hip replacement in 2003. My brain had conveniently helped me forget some of the realities of recovering from surgery. And it turns out that with a knee replacement there is a specific symptom of sleep interruption that didn’t come with any of my past hip surgeries.
Arriving at hospital, getting into the gown, and chatting to the anaesthetist and surgeon all felt very familiar territory. The mild anxiety of waiting (although I was lucky and first up; so down for surgery just after 8am) was also familiar. I had expected a spinal anaesthetic but to be sedated throughout, but the anaesthetist discussed with me the benefits of being awake; benefits for my recovery and also for not requiring an oxygen mask (a phobia from those childhood surgeries where you were ‘gassed’ to sleep with a big black mask). And so I chose to be awake. I can’t begin to describe the weird sensation of the table vibrating from the drill, and the sound and motion of a hammer on my knee, but without any feeling or pain. Yet it was interesting to hear the the consultant and his team discuss the exact angle they were going to plant the knee – 1 degree this way and so forth – until they found the right place. There was a fear that my still dysplastic right hip might make it hard to find the centre of rotation, but it didn’t.
I was also allowed to take my phone into surgery and listen to music – so my surgery was to the accompaniment of music by Bach, Holst and Vaughan Williams. I steered away from choral music so that I didn’t start singing!!
Recovery was very quick on day 1; I was still pretty numb so pain-free and without the anaesthetic I was able to eat quickly and importantly, for a Yorkshire girl, drink plenty of tea :-)
And then the pain started through the night. And with it, the insomnia. Now, I’m used to surgery and the fact that painkillers are required to get me through the early stages, especially at night. I had been warned that a knee replacement is much more painful than a hip and I can 100% confirm that’s the case. After my hip surgery I was able to sleep between pain meds; this time, not really. With today’s modern technology (a fitbit) I can tell you that on average, I had 1-3 hours sleep that week. And that sleep interruption still continues. I’m told that it settles after 3-4 weeks and I’m really hanging on for that because it’s so draining. I dream of the day I get into bed and feel my body relax rather than tense.
Thankfully, in hospital my days had a rhythm dictated by others - punctuated by times to take drugs, times to get up and mobilise with the physio, and mealtimes.
After four nights it was a joy to come home, to see my partner and my cat, and to be back in familiar surroundings. The first two days were really hard; after one night of my not sleeping, we ordered a spare bed for the dining room so my partner can, at least, sleep through my insomnia. It took us two days to get into a rhythm of how to wash, when to do exercises, when to rest, when to walk around, when to sit with a bag of peas on my knee to reduce the swelling. Since Monday we’ve figured that out more, and it is easier to cope within the schedule we have created.
Yesterday was an interruption to that schedule. I was back at hospital having my staples removed (quite painful I have to say) and seeing the physio. The wound is still a little bit open, so I’m steri-stripped up, but it does feel lighter and more flexible without the staples.
So until the wound fully heals I need to be a little more careful with bending the knee for a few days (no more videos of me on my CPM machine until next week).
Walking with crutches is OK and I’m well-practised having owned a pair since I was seven. But I am challenged by the fact that I naturally hitch my right (DDH impaired) hip, rather than using it normally, and so it was clear in the physio session that there is some ‘unlearning’ to be done. My left side – subject to all the other surgeries – is not strong enough to stand on (I have never been able to stand just on my left leg). Getting up our Victorian stairs is fun – I’m supposed to lead with my left leg, which I have never done in my life, and sometimes if I’m tired my partner has to push it onto the step for me. The joys of being differently-abled and where the bio-mechanic ecosystem that the new knee is fitting into is not in any way normal!
Every day some little things get a bit easier. And for that I’m grateful. I’m also grateful for an amazing partner who is able to be at home with me and shows enormous love and patience in looking after me, and being my carer as well as my boyfriend. I couldn’t do this without him.
Love to him and to you all xx
Jill Pringle was born with bilateral hip dysplasia (DDH) and has had a life of surgery including open reductions, leg lengthening, a hip and knee replacement. She writes to raise awareness of her different-ability and to raise money for Steps Charity who support people who can’t take walking for granted. You can donate here. Just £5 provides and information pack for someone newly diagnosed with hip dysplasia and their families.
Taking Steps by talking DDH
Steps Charity recently asked me to do a podcast interview as part of their new series which tells the stories of people like me born with all sorts of lower leg conditions. Click here to have a listen - none of it was edited, it’s just me sharing off the cuff what I do and don’t remember about childhood surgery for hip dysplasia, about having a hip replacement aged 32, and about living life as a differently-abled person who can’t always take walking for granted but lives a very active and normal life.
What strikes me most about Steps is how grateful parents are to have them to turn to, and the wider community of other parents they facilitate online. I talk a lot in this podcast about how reliant I am now on what my parents could tell me years later, and how their only source of information was what the medical staff told them in an era pre-google or social media. Consequently, I feel like I know the gist of my early surgeries but not the full medical details. In some ways it doesn’t matter – what’s important is that the surgeons at Sheffield Children’s got me walking somehow despite how much of my pelvis and hip socket was missing.
This podcast also helped me share some of my earliest memories of being in a hip spica plaster cast - what that felt like and how often we had to re-plaster my knees! I remember my childhood as very happy one, I had a mindset to try and do as much as what other kids my age could do. Whilst I couldn’t excel in sports I did well at school and as a musician, and consequently I’ve lived a very full life so far. My life has been punctuated by surgeries at different points and as you know, I am now waiting for a knee replacement in January – this time on the right side which has borne too much of my weight for almost 50 years. More on that soon!
Hope you enjoy listening to the Podcast. Link again here.
And if you do enjoy it, maybe you could drop a fiver in the pot for Steps here - £5 would help them support more people like my mum and dad with an information pack that says “you’re not alone and your child can have a good life with hip dysplasia, here’s what you need to know and the support that’s here for you”
Thanks for listening! xx
Hips, Knee and boomps a daisy!
You may have noticed that I haven’t been posting many walks recently. That’s because I’ve been finding it harder to walk any distance. I can walk, say to the swimming pool, or for half an hour along the river and back, but that’s about it. This year my unusual gait has become more pronounced and I feel less stable. I find it hard to stand up and sing properly – to firmly root myself in a comfortable position to support my voice. And I’ve been having more trips to the osteopath to re-align and reduce the pain in my upper body and head.
It feels like something has changed in the way I’m held together.
It has been four years since I last saw my orthopaedic consultant and over 19 years since he performed my total hip replacement. So this week I went along for a consultation and x-rays expecting to discuss hip revision surgery. The plastic liner to the joint wears over time, just like cartilage does in a real joint, and causes abnormal motion - and so I expected we’d reached the point where that, or other parts, might need replacing. I was pleasantly surprised to see from my x-rays that there has been very little change in the last four years (even after completing the South Downs Way in 2019) and the revision will be a future challenge.
The curved ball – or knee to be precise!
The issue with my current walking it seems, is my right knee. Nearly 50 years of bearing more than its fair 50% share of weight and compensating for the surgeries on my left side, plus dealing with the unusual shape of my right hip (my hip dysplasia is bilateral) and my crooked pelvis and different length legs, has taken its toll. The outside half of my right knee is now totally arthritic (with no gap between the femur and the tibia above and below it) and it’s veering inwards to try and compensate). So in short, I will need some sort of partial or full knee replacement on that side. My consultant is referring me to a different specialist to see if a partial knee replacement is possible, or whether I need a totally new knee. And to have more physio in the meantime.
Whilst my right knee has always been a bit painful, I hadn’t expected this diagnosis. I have always known that I’d need several hip surgeries throughout my life; it’s an expected part of the Jill plan. A bionic knee wasn’t on my radar. And it’s taken me a few days to get my head around it.
Funny what first flashes into your head isn’t it. My first question was “so how will that work on crutches then when it’s the side I rely on that will be in rehab and the side I can’t bear much weight on that I’m trying to rely on?!”
My whole brain is wired to rely on the right side and have surgery on the left.
This all happened the day I returned from a camping trip on the South Downs Way where I’d had the chance to ramble with my poles along a short stretch of the path I took two years ago. And in the week where the top sportspeople from the #WeThe15 differently-abled population are showing us what’s possible at the Tokyo Paralympics.
I know that I will work through this next challenge. I’m still swimming, still singing and still walking – just with smaller steps and bit more caution, for a while. I’m nearly half-way on my virtual walk – 130 miles down, 138 to go. Every step counts, however small.
Will I finish it before or after I get a new knee? I’ll keep you posted on that one xx
Jill was born with bilateral hip dysplasia (DDH) in 1971 and has had various surgeries including a total hip replacement. She walks, swims and blogs about hip dysplasia to raise awareness of this diff-ability and money for Steps charity. Follow @WalkingJill on Facebook.