Return to work: post-hip surgery
Three and a half months post my hip revision surgery was time to return to work. I’m very fortunate that I can do my job remotely, but it does involve a lot of sitting. With my hip dysplasia, and especially post-surgery, this is of course better than a job standing on my feet all day. But as anyone with joint issues will tell you, being too sedentary can also cause problems and become painful.
The company that I work for is understanding and I’m also able to phase my return to work, to minimise prolonged sitting. I’m working four hours per day to start with, and after some trial and error in week 1, I’ve learned it’s better to split those hours rather than try and work just mornings. Two hours at either end of the day allows me to balance moving and resting between working, which helps stop my hip seizing up, and gives my arms and neck a rest as they get used to life with a screen, keyboard and mouse again (think about how you have to adjust back to that posture after a two week holiday!). My home office is also next to the bedroom, so I’ve found it helpful to be able to have some video calls sitting on the bed, with my legs out in front of me. This distributes the load on my hips differently and the variety of positions between chair and bed, makes it easier for me to focus on my work, not my body.
It’s been good to get back into the rhythm of working. There are only so many eps of Love it or List it that I can watch, and it’s good to apply my brain to something other than my own rehab. The best part has been meeting colleagues again, and especially my own amazing team of marketers; their passion, drive and humour has been energising. And I have a purpose each day. Plus the weekends are actually different from the weekdays.
So now, it’s about settling down into this new rhythm, whilst making sure that I use my ‘off’ hours, to keep up my exercises to improve my physical capabilities. The first week I worked on 3 days, which was enough! I slept a lot that weekend. By day three, my hands had started tingling, two fingers a little numb. We think this is a combination of thoracic outlet symptoms and the carpel tunnel being aggravated by my crutches. And so I’ve got some different crutches to distribute the weight across my whole hand, which is way better.
Last week I worked on 4 days, with Wednesday off to rest and do physio. Splitting the hours definitely helped with the tingling. And…drumroll…I finally made it back to the swimming pool - yippee!!
Swimming has always helped my upper body, which I over-use to compensate for my weak hips, glutes and quads. So when my upper body symptoms started, I knew I had to try and get in the pool. The staff at the local health centre know me well, and were brilliant as ever. As was my partner who came for moral support/backup the first time.
Amazingly I could get in and out of the pool via the ladder (relying on my right leg to take most of the weight). The only challenge is where to put the crutches, and more importantly, how to pick them up when I get to the the top of the ladder. The answer is to ask another swimmer or lifeguard.
Being in the pool made me smile from ear to ear - literally. And as I took those first few strokes (strictly front crawl) my neck, arms and lateral muscles were smiling too. Finally they get to move freely, not hold solid. I alternate between swimming, and doing hydrotherapy exercises. Which also means my partner no longer has to drive me to hydro sessions, which saves a couple of hours a week. I can walk to and from the pool and because my return to work is not yet full time, it doesn’t matter it takes me 25 minutes each way (ordinarily it’s about 7 minutes) in the middle of the day. I can also swim and navigate the changing rooms when it’s quieter, instead of early morning.
It’s still going to be some time before I see the full benefit of this surgery (a whole year according to my surgeon).
So what can I do? I can now sit on a normal height dining chair, as long as it has arms, for about 30 mins. I still can’t consider a sofa. I’m back to sleeping upstairs my own bed. And with the help of a bath board and an extra grab rail fitted above the bath, I can make it into the shower. I am not missing the daily flannel washes! I can walk around the ground floor of the house with one crutch, so I can carry a cuppa from the kitchen to my armchair (important for a tea addict). And when I’m out I am much more confident walking with reciprocal crutches, taking a bit more weight through each leg, and using a more ‘normal’ gait.
What can’t I do, yet? I still need a slightly higher loo seat with arm rests, so I can’t brave being away from home for long enough to need a pee. It’s definitely easier getting into the passenger seat of the mini, with only 2 cushions now needed not 4, and I can lift my own leg in and out rather than needing help. But I can’t close the door behind me as I have to have space to open the door really wide. And I can’t sit well enough to drive even the automatic car. A train or bus trip feels some way off. So no singing in carol concerts this Christmas, alas.
But still, I am making progress. I have come a long way since my hip revision surgery. And with the bilateral hip dysplasia and other odd joints, it was never going to be a speedy recovery. But returning to work, and to swimming, are both big steps on the hip revision rehab journey.
Thanks for being with me and sharing my progress.
Love, Jill x
Jill Pringle was born in 1971 with bilateral hip dysplasia and has had various orthopaedic surgeries as a child and adult. She writes this blog to share her experiences of living and walking with DDH to raise awareness of this common condition. Jill had a full revision in 2025 of her hip replacement from 2003.
The specialist therapy jigsaw for hip rehab: physio, hydro, podiatry
It’s now 9 weeks since my complex hip revision surgery. In the last few weeks I’ve seen various therapists who each deal with a different part of the rehab puzzle: Physiotherapy, Hydrotherapy, Podiatry and Chiropody. With a lifetime of hip dysplasia, bringing this together requires a slow and steady approach that’s a lot more tortoise than hare….
Physiotherapy
I’ve been seeing a physio every 2-3 weeks since my surgery, and physio is definitely the centre of my recovery plan. Whilst the surgeon sets the guardrails around my rehab (the pace and limits to protect the hip whilst it stabilises) it’s my physio who I see as the key person guiding my progression. More recently my exercises have been about getting specific muscles to engage that will restore particular day to day movements; sit to stand, sliding and lifting my leg independently, stepping up and down, bending my hip fully to 90 degrees in some positions. And walking reciprocally with my crutches (mimicking a more natural way of walking and taking more weight through my operated leg).
I found this physiotherapist over 15 years ago and her knowledge of how different my ‘baseline’ is to a normal set of hips and knees has been critical. She also gives me advice for hydro and podiatry and I let them all share my personal data/liaise if they want to.
Hydrotherapy
After my last post-op consultation I was allowed to start hydrotherapy. This is both a relief (I’m a swimmer and I’m really missing the water) and extremely tiring. My first session was overwhelming, both physically and mentally as I was so anxious not to do ‘too much’. I had my second session yesterday, which was much better because I knew I’d been OK after the first one. But still tiring - I slept so well last night and I’m sore today. I always progress faster once I start hydrotherapy because the support from the water (and so being 50% not 100% weight bearing) means I can make more movements for longer - stand/sit, walking, cycling movement, leg raises etc. We are being a little cautious about some movements like abduction, and not adding resistance like flippers yet. But I can do so many more repetitions of my exercises in the water. Plus I get a proper shower at the end, which still feels like a luxury until I’m allowed to step into a bath to take a shower at home.
Podiatry (orthotics)
I first started with orthotics a few years after my initial hip replacement. My knees, ankles and feet are all part of my unusual biomechanics - none of them are ‘normal’ and there’s a lot of hypermobiity (ie they’re loose, so add additional instability to way I walk). Post my hip replacement, I got some custom orthotics for the first time in both my shoes - to help correct a small (1cm) leg length discrepancy, and to help stabilise the position of my knees and feet when I walk. After my right knee replacement, the leg length discrepancy became more acute (more like 2.5cm) and so for the last 3 years I’ve had an outer shoe raise as well as inner orthotics. It’s amazing what can be done by a good practitioner (gone are the days of the big black surgical boot).
After my recent hip revision surgery, my new metal hip socket is a bit bigger and less worn, so I’m back to around 1cm difference again. It will take about one year of continuous improvement before we know exacely where it will end up - so I don’t yet want to spend money on a new permanent solution (custom orthotics aren’t cheap).
So, last week I saw the podiatrist (who I’ve also been working with for a number of years) for an interim solution. A couple of ‘shims’ to about 8mm (think thick bits of insole custom cut to size) under my most recent inner left orthotic, has allowed me to remove the outer shoe raise. I’ve only had this solution for three days yet I can already feel the difference - the position of my left knee and ankle when I walk is much straighter and more stable. This will become really important when we get to walking without crutches, and right now, it helps with physio exercises like sit to stand from a chair, because my knee can take more weight. My hip muscles are a little sore as they adapt to a slightly different (correct) use of the muscles, which have all been traumatised by the surgery.
Chiropody
Not an obvious essential therapy, but when you’ve had any hip surgery, by far the hardest thing for a very long time, is reaching your feet! Putting on shoes and socks needs assistance, and cutting your toe nails is just impossible. Comfortable and healthy feet are essential when you’re re-learning to walk. So my trip to the local chiropodist this week felt like a birthday treat!
Putting the puzzle together, more tortoise than hare
Major and complex hip surgery - something I’ve had more than once in my life due to my hip dysplasia - takes a long time to fully recover from. In fact, physio and conscious monitoring of how I walk and move is just a way of life and constant progression.
A tortoise, not hare mindset is important! Slow and steady, piece by piece, rebuilding movement, range, strength and stamina is a very particular sequence, guided by experts. Two days after my op, having orthotics managing my knee position was not as important as just getting me mobile on crutches. 9 weeks on, if I want to progress further, it is important. Because my knee not my hip was beginning to limit what I could do.
Every time I have surgery I’m amazed by how it does come together, bit by bit, with the guidance of experts and me diligently doing what they ask every single day. Every time I’m impatient for quicker progress (not a naturally patient person!). I have to work hard to calm my ‘inner hare’ and keep the tortoise moving forward. Tortoise Pringle will win the race and it was never going to be a sprint!
Thanks for reading and supporting my progress. Love to you all x
Jill Pringle was born with hip dysplasia (CDH/DDH) in 1971. She had several hip and leg surgeries at Sheffield Children’s in the 70s and 80s, and as an adult has had a left total hip replacement, total knee replacement (opposite side) and most recently a full revision of her original hip replacement. She writes about her surgeries and has also undertaken various walking challenges, to raise awareness of hip dysplasia. You can listen to more of her story on the podcast here.
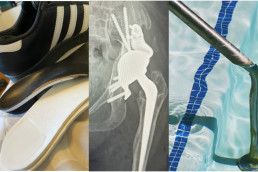
Before and after hip xray: hip replacement to hip revision
So here is my new hip! With a handy before (hip replacement) and after (hip revision) comparison Xray. First thing that strikes me is that there’s a lot more metal than pelvis now. Due to my hip dysplasia, I’ve never had much pelvis on that side (which was the difficulty with getting my childhood reduction surgeries to stick). The challenge for the hip revision was to extend the socket and so that bit you can see on the right hand side of the Xray is the custom 3D printed metal socket doing just that job.
I was talking to a friend a few weeks ago about the fact that I was finding it difficult to visualise my new hip because I hadn’t yet seen an Xray. And in that conversation it became clear how much I understand my condition through the hip Xrays I’ve had through my life. I have never not had a mental image of what my pelvis and hips look like and I suspect that’s the same for anyone diagnosed with CDH at birth. And so I suddenly felt lost. Now, I ‘get it’. I can see what my orthopaedic surgeon has done and I can finally connect the image with how it feels. It’s reassuring to me.
The last few weeks have been very boring. I’ve been diligent and consistent with my physio exercises, and maintaining all the restrictions around precaution height and restricted movements. For the last 3 weeks I have at least been able to go for longer walks on my crutches, but I still can’t go anywhere where I need to sit.
I saw my Xray when I had my 6 weeks post-op check up this week with my orthopaedic consultant. He seemed pleased with my progress - wound is healed well, no infections, no thrombosis, nerves appear to be undamaged and the leg is “pointing in the right direction”. He was also happy that I’m taking things slow and steady - something he wants me to continue for the next 7 weeks. I am still to stay on crutches as by far the biggest risk is falling. As he said, in essence it’s like having a big fracture in my pelvis and that needs caution. I guess if I fall and damage this, there’s no more pelvis to play with, and now I’ve seen the Xray my brain gets that so much more.
So it’s more of mostly the same.
- I asked if I can swim yet, we compromised on me adding supervised hydrotherapy into the mix, as long as I take it carefully.
- Continue with the physio with the advice of take it slowly and carefully.
- I can however start to play with lowering the precaution height of chairs very gradually - eg removing one of the three cushion - as long as I never bend more than 90 degrees. As this progresses it will give me a little more freedom to at least walk further if I can sit on a bench or in a cafe to rest half way.
- Still no bending, twisting or climbing into the over-bath shower though….so still the strip wash regime continues into September. At least when I go for hydrotherapy I’ll be able to have a shower afterwards - can’t decide if I’m more excited about getting in the pool or having the shower!!
If I'm honest, I had mixed feelings after my appointment. Obviously the overriding positive feeling is that I’m progressing well in his expert eyes, and that surgically he is considering this a success. But I also had a feeling of dashed hopes. Hopes that I could start to do more, more quickly - particularly swimming or driving, which would give me more independence.
But this is not my first surgery and I know that by sticking to what I’m asked to do, the end result will be more positive. This too shall pass. And my independence day will come :-)
Meanwhile, stay tuned, thanks for following. Love to you all x
Jill Pringle was born with hip dysplasia in 1971, in Sheffield (then called congenital dysplasia of the hips). She's had many orthopaedic surgeries as a child and adult. Jill writes this blog to share her challenges with walking as a differently-abled person.
Post-Op recovery: 1 month milestone
It’s one month today since my hip revision surgery. I find this week 4-6 period of post-op recovery the most boring. The first week is mainly feeling ill and getting over the trauma. Weeks 2 and 3 are about getting more mobile as the swelling and pain subsides; balancing movement with rest. But the second three weeks can drag - I no longer feel ill, I’m not in a lot of pain, but I’m still really restricted in what I can and can’t do. My exercises are still quite restricted, I have to vary my sitting position too regularly to sit in one place for any length of time. And there's not much variety in the days. It's the boring phase!
For those who haven’t read a previous blog post, I had a full revision surgery of my 22 year old hip replacement, one month ago. I’ve had 13 surgeries all due to being born with bilateral hip dysplasia (CDH) with one hip socket missing along with a lot of my pelvis. You can listen to more of my history on this Steps Charity Podcast here.
So what am I up to every day?
Walking, always with crutches.
As well as continuing to march up and down the garden, I’m now also taking a walk around the block each day, on crutches. Walking is by far the best PT for post-op recovery. The surgeon was strict about using crutches for eight weeks, even indoors, and to date I’ve been using them together (ie both crutches go down together as I take weight on my operated leg). As of yesterday, my physio has added a small amount of walking in the garden using the crutches reciprocally, which means a bit more weight through each leg, and a bit more of a natural walking pattern. Sadly, I still can’t walk to the local cafe, as I can’t then sit down (chairs not high enough to meet the precaution height). Nor am I braving the local coop as there are too many ‘hazards’ like people, wet or uneven floors, baskets etc to feel safe. But the daily walk is enjoyable, and extends my bubble beyond the home.
Physio exercises, with some progression.
After a hip replacement you get one NHS physio appointment for post-op recovery and a pack to follow a standard progression plan. So I decided to use a private physio who has worked with me for the last 20 years. She knows my history (so we’re not starting from scratch with me having to explain how different my hips are). She also knows who my surgeon is and how he likes to work. And most importantly, she knows all the ways I can find to ‘cheat’ the movements I find most difficult! Over 50+ years I have become very creative in this regard, but that gets in the way of me exercising the muscles that actually need to learn to work properly. For someone like me, with a complex case, it’s important that the physio doesn’t expect to do much that’s standard, and can be bio-mechanically creative - ie find different positions or props that help me exercise the right muscles safely.
For the last two weeks exercises have been:
- Standing: Heel flexes, Hip abduction, Hip extension, and then standing on my operated leg (with crutches) and moving the other one into various positions (looks like an odd tap dance!) - so that I get comfortable with the left leg taking the weight and encouraging independent movement of each leg.
- Laying: knee/hip bends, hip abduction with knees bent, hip adduction with knees bent (pushing on a rolled towel) and pelvic tilts with knees bent (but still NO bridging allowed).
For the next 3 weeks this has progressed to:
- Laying: hip abduction and pelvic tilts
- Sitting (new position puts more weight through the hips): leg extensions and holds with ankle weights, hip adduction (squeezing a towel between my knees which works the glutes more sitting than laying, and standing from a perch position without using my arms (REALLY hard!)
Short bursts of reading, watching TV, writing, learning to paint :-)
It’s important to keep my brain busy. But I have to be super careful not to sit in one position for more than about 40 minutes. So things I can do in short bursts are good, where I can also switch position between my high seat chair vs. the bed with legs up. I was never an artist at school (I’m very literal, and my creative outlet was always music) but I’ve bought a small watercolour set and a book which is helping me learn to paint natural things like leaves and flowers. Don’t expect the gallery opening any time soon folks! But it’s a very relaxing thing to do.
Visits and calls from friends
I’m very grateful for everyone who has visited or arranged calls/zooms. It’s lovely to see people, hear about things other than my boring little daily routine, and just laugh and enjoy the company of people who I know well. It also adds some variety to my day and means I will still have some social skills by the time I go back to work or choir in the Autumn.
So these are the things, day-in, day-out, that stop me from getting too bored - which would lead to my doing too much, too soon. My surgeon has put the brakes during this initial period of post-op recovery for good reason. So I need to trust in that, until I see him in two weeks' time. Hopefully then I'll find out that everything is going OK and the new hip will have ‘set’ enough, with new bone forming to hold it in place securely. Then, hopefully, the handbrake will the released a bit to allow proper rehab to start - including hydrotherapy. And I'll be rewarded with a chance to see an Xray of my new hip for the first time - Xrays of my hips have always been how I understand and connect with my hip dysplasia.
So until then, thanks for reading this and for following my progress. Stay tuned for the next episode in a couple of weeks xx
Jill Pringle was born with bilateral hip dysplasia in 1971 in Sheffield, UK. She has had various childhood and adult surgeries on her hip and knee. She writes this blog to raise awareness of living with CDH/DDH and being a ‘differently-abled’ walker.
Hip revision precaution height: managing at home post-surgery
It’s two weeks now since I came home from hospital after my hip revision surgery (all due to my hip dysplasia). In some ways time has flown, in others it has dragged. It’s a bit like Groundhog Day; punctuated by exercises, napping, walking on crutches, eating, washing, a bit of TV, a para of the blog and then start again.
What marks out a hip revision surgery is the need to restrict certain movements until the hip socket sets in place securely. So that the screws holding the socket into the filler in the pelvis set. Big movements are a big no. And I have a strict precaution height.
The restrictions are:
- No walking without crutches. To limit my movement and weight-bear sensibly
- No flexing the hip to 90 degrees plus. So I can’t sit on a chair, bed, toilet lower than 47cm (18.5 ins) - my precaution height.
- No twisting or rotating in a way that could allow the ball to slip out of the socket. So no low chairs, no squatting and no stepping in and out of a bath. Flannel wash only for 6 weeks!
- No sleeping on my side even with a pillow between my knees. It is difficult to sleep in the same position all night, but I can only sleep on my back.
- No crossing my legs.
- No hip-bridging exercises. All the physio exercises have quite a small range.
- No driving and extreme caution getting into and out of a car to manage precaution height. We have a mini so this has been fun!
All of the constant thinking, minding how I’m moving, is mentally tiring.
What is a precaution height?
Put simply, the precaution height is the lowest furniture you can sit on. It means you don’t end up flexing the hip too deep when sitting, or standing up from a seat, and so don’t risk the hip dislocating (painful) and then weakening the fixings.
It’s calculated based on the height of your knee to the floor when sitting in a chair (you make the measurement before surgery).
Most dining chairs are about 40cm high. Sofas and toilets can bit lower. I also need arms on anything I’m going to sit on, so I can take the weight on my arms and lower or raise myself up whilst protecting the hip and keeping the leg straight.
This led to me purchase things for home before surgery, like a high seat chair with arms, a raised toilet seat, and a second hand single bed that’s quite high from the ground.
The hospital also sent me home with a loaned sit/perching stool for the bathroom so I can sit at the sink and wash, or at the kitchen counter to make a sandwich. A Leg-Up leg lifter, so when I slide back onto the bed, I have a way of pulling my operated leg round. A sock buddy (weird contraption to pull on socks, which so far has been usurped by boyfriend LOL!), and lots of grabbers to pick things up.
Pain and bruising
The first few days home I was still on power painkillers because I had breakthrough pain from the incisions, the nerve disturbance, and the internal bruising. These also helped me sleep, especially when first in bed. But they do contribute to nausea and dizziness and I don’t need more of that post-surgery!
After three days I’ve been only on paracetamol and ibuprofen, and I would describe it as mild pain and discomfort. Doing my exercises was sore until the bruising and swelling reduced - this subsided after about a week, so 10 days post-surgery.
And I’m on blood thinners, to ensure I don’t develop clots, until the end of July. Which means being super careful not to cut myself or develop any new deep bruises.
Sitting in a chair or perching on the stool was difficult for the first week. Then each day the swelling reduced - it was like an extra bit of my sensation returned. Right now I can can still only sit for about an hour before I have to move due to discomfort. When I first got home this was 15 mins.
The incision/wound
I had the wound checked yesterday by the local GP nurse. It’s all looking clean and healing well (they went in using the same anterior scar from my hip replacement 22 years ago). Thankfully no staples to remove like I had with the knee, just self-dissolving sutures.
What’s worse - hip or knee surgery?
The pain from the knee replacement was 10x that of the hip revision. Those first three weeks of throbbing pain and the lack of sleep for 3 weeks I hope never to repeat. By comparison this hip surgery has been child’s play - pain-wise.
Howvever, the movement restrictions from the hip revision are more limiting right now. I could do more (pain aside), more quickly, with my knee. I didn’t have this 6 weeks of restrictions. So the hip revision is going to take longer to recover from.
Physio exercises
By far the exercising is walking. Weight bearing (with crutches) to build strength and encourage new bone to develop is part of the PT routine.
For the first two weeks I had a few exercises, each with limited range;
- laying: ankle holds, quad holds (pushing my knees back into the bed), hip bends (sliding the heel up to bed bending the knee), buttock squeezes - definitely sore for the first week! Plus straight leg hip abduction which I have never been able to do easily without help.
- standing: hip abduction, hip bend (lifting the knee a bit), hip extension (leg back), and heel raises up to tip toe.
- sitting: seated knee extensions for both legs, strengthening the quads
I’ve been doing these religiously 3x a day. And it’s amazing how much easier they get once my body (and brain) is trained to do them. A marker of progress. Little victories.
Always followed by an ice pack to relieve the pain/soreness from doing them.
Friends on rota - thank you!
After one week home my partner had to return to work (for a rest, LOL) and I’m grateful for the friends who came in on rota that first long weekend, to break up the day and help me. I express just how lovely it was to see you folks; for the lunches, the cuppas, the hair washes, the washing hang-outs, the plant watering, the cat feeding and basically just letting me live vicariously by hearing about things other than my regular Groundhog Day existence.
Of course the biggest thanks go to my loving and patient partner and my emotional support cat. I can’t imagine the last two weeks without them.
And to all of you out there reading these posts, and sending good wishes, thank you and love to you all. Until next time... xx
Jill Pringle was born with bilateral hip dysplasia 53 years ago. She writes this blog to share her experiences of living and walking with this condition, and about her adult and childhood orthopaedic surgeries. Jill is also a proud differently-abled supporter of Steps Charity, who help children and adults who can't take walking for granted.
Post-surgery hip mobilisation and the get home checklist
Restoring independent mobility is a priority after hip surgery. Hip mobilisation reduces the risk of blood clots or chest infections and our joints and muscles were designed to move. But before you can get up it needs to be safe - the sensation needs to have fully returned to your legs, and you need to be strong enough to stand without the risk of falling. In short, being a Fainting Freda is a barrier to achieving this :-)
Fainting and sickness
The day I had my knee replacement 3 years ago I was using a walker the same afternoon. I wasn’t sick because I was awake with spinal pain blocker and very light sedation only.
But for my hip replacement 22 years ago, it took 3 days to get me out of bed due to the sickness and fainting I experienced post-general anaesthetic. My friends all know that where alcohol is concerned I’ve always been a total ‘shandy lightweight’. A couple of glasses of wine on a night out and I’d start puking, and my hangovers were fierce. My body just doesn’t tolerate toxins. So anaesthetics are not tolerated well either. All through childhood surgeries, a lot of vomit was an accepted part of the recovery.
So for my hip revision surgery nearly 2 weeks ago, I wasn’t sure what to expect. I wasn’t having a general, instead they used an epidural pain blocker, but unlike me knee replacement, I was fully sedated. What happened post-revision was more like the hip replacement, with the sickness and fainting, but nowhere near as bad on the sickness. For which I’m thankful.
I was sick twice in the early hours of first morning in PACU, but fast acting anti-emetic injections stopped that. The following morning they tried to sit me on the edge of the bed, but with the epidural still attached, and a catheter still in, I was quickly put back into bed for a bed bath. After breakfast at 930 the epidural was removed along with the arterial line, and by 10am I was wheeled down to the ward in my bed. My legs were not fully thawed, my non-operated lower leg taking the longest to return to full feeling. Hip mobilisation was going to take a while.
Meanwhile, I’m watching everyone else get up an about on crutches. My competitive side was not enjoying this! But I know from my first hip replacement I just need to go with it. My body takes longer. And my surgery was more complex and longer than average.
The first tentative steps on Day +1
At 3pm the physios decide it’s time to try and mobilise me. I move to the edge of the bed and then I’m up and walking a few steps on a walking frame. My new hip feels really heavy and stiff, because it’s swollen. But boy does it feel good to move - physically and psychologically. The physio moves me back to sit in a chair, at which point I start to feel dizzy, and I say “I’m going to faint”. The nursing staff were there fast, I was given oxygen, they kept me focused and conscious. They managed to get me to take the few steps back to the bed, where they could tip the bed back to get more blood to my brain. I didn’t actually faint… so this was progress, but my blood pressure had dropped. The 30 degree heatwave outside wasn’t helping, so they brought me a big fan which is now a static feature by my bedside even at home.
Despite all that, the first night on the ward was quite relaxing all things considered. A nice dinner, chatted to the two other ladies in my ward, and we all read our books until lights out.
Out of bed with some anxiety on Day +2
The nurse assistant got me out of bed and into a chair after breakfast, and I didn’t faint which was a good start. Sitting for the first time felt strange and uncomfortable, but then sitting is not that comfy for me generally. My pelvis is very crooked, and so I can never quite sit straight. But I managed to wash with the help of a long handled sponge, and put on my own nightshirt. Another step towards independence. At this stage in recovery, doing one new thing seriously feels being let out for a night out in Vegas. But I also felt vulnerable in the cubicle. What if I faint and break my new hip? What if they can’t get to me?
I waited for the physios whilst watching the 84 year-old who had her surgery last night get up onto crutches, go off and do the necessary hip mobilisation checklist, then she started packing to leave. It was my turn, first up on the walker again, and then onto crutches. Now, with my history, I’m a dab hand on the sticks, even if I do say so myself! All looking very impressive.
Later the physio came back and I was straight up onto crutches. Yay, look at me, so confident. Star pupil. This feels good. And then, yep, you guessed it, I say, “I’m feeling odd, I think I’m going to faint”. We get back to the bed, she takes my blood pressure which has tanked again, and so I was back in bed and on a drip of fluids. Which to me, was a backward step. I shed a few tears as the physio said no more PT today.
My partner came to visit and brought some lovely messages from colleagues and friends who he’d updated (thank you, they were well timed folks!).
After he left, I lay down and figured out the pay as you go TV. I needed a distraction. Then the nurse came with my blood thinner injection (which is the least painful needle ever really) and I got really anxious. All I could think was - oh no, the cannula made me faint. I got quite upset. He was very patient, let me have my mini-meltdown, then gave me the jab. I settled back to watch Speed (Keanu always helps right?!) whilst taking on the fluids and the breeze of the fan. Watching a movie felt normal and it was the distraction I needed.
This was the longest night. I didn’t sleep at all, the next patient to arrive in the bed opposite was struggling with pain and very vocal, and I almost fainted again when trying to use the loo. So back on the drip, the fan. Was I ever going to get home?
Day 3 - the checklist to get home
It was Friday and I wanted to get home for the weekend. I felt like crap but recognised I needed a plan, and I needed to feel in control. So I started asking the day staff - what do I need to do to get home now?
There were four things:
- Not faint/nearly faint
- Bowel movement and pee without the catheter
- Have an Xray
- Fully mobilised on crutches - on the flat, up a single step, and up and down a flight of stairs
So I had a goal and a plan. I’m good with that, and the fact I asked in itself showed I was ready. I focused on each with determination.
After washing myself in a chair the catheter came out, which made it easier to get up and mobile (dragging a catheter bag around on crutches adds something extra to think about)
The physio got me up and I walked down the corridor on crutches and up and down a single step. I found this easy - up: good leg, crutches, operated leg. Down crutches, operated leg, good leg. When we got back to the bed the physio asked if it was my goal to get home today? You bet it is!! The ward staff said OK, if I could toilet independently.
Shortly after I went to Xray in a wheelchair. I haven’t yet seen the image of my new hip joint, and I’m very curious to see it. I will have to wait until I see my consultant orthopaedic surgeon in 6 weeks.
After lunch, with a bit of extra medicinal help and focus, my bowels finally opened. Poo for victory!
Then the physio took me up and down a flight of stairs, which I already knew how to do. We did my standing, sitting and laying mobilisation exercises so I was clear on them. And proved I could get on and off a raised toilet seat on my own.
We don’t have a walk-in shower at home, so have to strip wash only for 6 weeks (the risk of bending or rotating the hip too far is to big). So I had a sneaky shower in their wet room. Such bliss. Clean hair, the feel of water on my skin. Post-surgery these little moments are so precious. I felt human again.
I then waited for the discharge papers, the sick note, the meds - with the hospital transport already waiting to take me home (we have a mini which won’t easily meet the precaution height of 18.5 ins). Then I was cleared to go. Yippee!!
I was soon cleared to leave, considered fully mobilised. We had to faff a bit with the wheelchair to get me downstairs as it didn’t meet the precaution height. Lots of pillows. It was hard to get into the ambulance, but we managed. It was a 40 min journey, which I shared with a lady who had just had her knee wound staples removed (ouch, remember that one). The ambulance had limited suspension to we felt every speed bump, and the air con couldn’t keep up with the heatwave. But at 5pm, I pulled up at home.
Thankful for home
My partner was there to meet me and with the help of the ambulance driver we got up the two steps. My partner set up a bed for me downstairs, so I have everything I need on one level and don’t need to climb the steep Victorian stairs. Dudley the cat was a bit unsure for a while, but soon came for a cuddle. Another very happy moment.
We ate dinner. We watched an episode of something on the TV (I could sit in a chair for about 30 mins before needing to move). Then got ready for bed. I have never been so thankful for home.
The NHS staff at SWLEOC are incredible. I will also always be thankful for them too.
We’re all differently-abled
As I reflect on this post-surgery mobilisation, I’m conscious that we are all diff-abled. No two people will mobilise the same post-surgery. Some of us just take a bit longer. But we get there.
Until next time, thanks for all the love and support folks xx
Jill Pringle is 54 and was born with bilateral hip dysplasia. You can read more about her experiences of living with this condition, and her various orthopaedic surgeries on this blog, or by following @WalkingJill on Facebook.
Hip Revision Surgery: my first day and night in hospital
I had my total hip revision surgery just over 1 week ago. It’s been a full-on week or so, as I start to recover from a major surgery.
This is not my first hip surgery. Born with bilateral hip dysplasia (DDH) in 1971, orthopaedic surgery has been a regular cadence throughout my life. As I child, I had several surgeries to finally get me walking by the age of 3 and a half, a femoral plate removed when I was 7, a leg lengthening surgery aged 16, a total hip replacement (THR) aged 32, a knee replacement at 50 and now this revision on my original THR.
I had my surgery at the elective orthopaedic centre (SWLEOC) at Epsom Hospital in June 2025.
The morning of surgery
I had to be at hospital for 7am and I’d been fasting since the night before. I had a big glass of water at 6am then nothing. I showered in the same special wash I’d been using for the last 3 days. Despite my hunger, the journey was calm and uneventful as my partner drove me there. Heading for major surgery is a weird feeling, not unfamiliar to me. I know it’s what I need, and have been waiting for it, yet it’s scary. All the what ifs and risks are bubbling under the surface, and just that feeling that I’m about to put myself through intentional pain and trauma is unnatural.
Along with 6 other patients, my partner and I were taken up to pre theatre. It was unexpected and reassuring he could come with me - my last surgery was just past covid so no visitors were allowed at all. It helped to have a friendly face there, someone who loves me. I gowned up, had the usual pre op checks to make sure I was fit enough, ensure no infections, scratches or bruises. They drew a big arrow on my leg and wrote LEFT on it for good measure!
The anaesthetist visited and explained it would be a spinal pain management with a sedative, rather than full general anaesthetic. For me this was good news - I have never reacted too well to the GA hangover. He inserted a cannula in my arm so they could take blood and to later administer the meds. He then listed all the side effects and risks, as they must for informed consent. And then something new happened. The room started spinning, I got dizzy and hot, and I fainted. Next I knew was my partner telling them I don’t like masks on my face, as I came round. It’s called a vasovagal response but to you and me, it’s fainting. It’s a common feature of my previous post-surgery journeys because my blood pressure is naturally low. But I’ve never done it pre-op before. First time for everything!
They put me back on the bed and I was quickly back to normal. The staff reassured me that it’s quite common and all good. My surgeon arrived, which was reassuring as he’s been my consultant since 2002. He explained the hip revision surgery again, showed me a diagram of the hip joint that’s been built, and said I was first up in theatre so not long to wait. It would be 4-5 hours and I might lose blood and need transfusions. He also reminded me it’s going to be a long recovery where I need to be slow and steady, not take any risks for the first six weeks, until the new hip sets in place. He confirmed I will be weight-bearing with crutches but need modified exercises due to the much higher risk of a revision dislocating and the need for the joint to set in place.
Before 9am I said goodbye to my partner, and was wheeled in a chair to theatre. The scene when I arrived was actually fascinating - like a scene from a movie, with lots of people in the background in blue hazmat style suits readying things! I recognised the anaesthetist team, who asked me to transfer to the operating table, undid my gown at the back, asked me to lay on my non operating side then hooked my cannula up to the drugs machine. “First anti sickness” says the anaesthetist. “OK now the sedative." I asked ‘should I be feeling sleepy?. He says yes. And that’s all I remember.
The afternoon - coming round in PACU
I think I remember them first bringing me round in theatre, I have an image of a few people in gowns/masks looking at me and saying hello, including the surgeon. The next thing I remember is being in PACU, with a two lovely smiley nurses, Pam and Suzy, telling me where I was and that they were looking after me. I was hooked up to fluids and they explained that I also had an arterial line on the other side so they can take bloods regularly to check my haemoglobin levels. They gave me my phone and I messaged my partner to say Hallo and sent a selfie, so he knew I was OK and could let my sister and colleagues know. This was at 2pm. The surgery had taken 4.5 hours.
Regular observations (obs) of my blood pressure, temperature, oxygen levels continued. I had some water, a cup of tea and some toast which was heaven. They asked me to wiggle my toes, see if I could lift my legs, and seemed happy. I had no pain, the epidural was still attached and would be all night. And then I almost, but didn’t fully faint, to add a bit of drama. Once again it was over quickly with some oxygen and a big fan (which has become a staple post-surgery friend for me).
The anaesthetist and my surgeon both visited me. They were un-fazed by my fainting - long surgery, lost some blood, I’m lightweight, and I’d been fasting.
My consultant orthopaedic surgeon explained that the surgery went to plan, so he was happy. He reminded me it remains very fragile in there - I have so little pelvis on that side in the first place to work with. And he reiterated no risks at all, slow and steady for 6 weeks, just focus on letting the bone and metal joint bond so it gets nice and secure. He reminded me only to walk with crutches, no twisting, carrying, crossing my legs or over rotating the hip, and be hyper-aware of my precaution height - the lowest furniture I’m allowed to sit on so I don’t end up bending to to 90 degrees or more. More on this in a future blog because, frankly, it’s quite limiting!!
My partner came to visit about 4pm. I heard him coming down the corridor, and it was the happiest thing to see his face and get a big kiss. It was lovely to chat, although I expect I made no sense whatsoever (nothing new there he’d say!!). He brought pics of Dudley, our cat, saying hello :-) I had sandwiches and a protein shake.
Obs continued throughout the evening, once my legs were better thawed they hooked pain meds into my epidural. Then I was sick so they gave me anti sickness injections and fluids. They had to keep spraying my legs, waist and trunk with an ice spray, to test what I could feel below and above my waist whilst the epidural was still in - to make sure that any spinal pain relief was not creeping up my body as that could impact my breathing. The regularity of my obs was a reassuring drumbeat.
The evening - a long night of intermittent sleep, pain, meds
As the evening progressed, many of the people who were in the waiting room with me that morning were mobilised up onto crutches and left either to go home, or down onto the ward. I remember this from my first hip replacement where as the youngest (but also the most complex) I had taken a few days to mobilise whilst all the 70+ patients were whizzing around on crutches on the same day!!
That first night I stayed in PACU. I had a new nurse called Andrew overnight who looked out for me and a couple of other patients all night. With regular obs, ice sprays, anti-sickness and other drugs, and the fan on all night to help keep my temperature stable. My legs slowly thawed - ironically it was the non-operated leg and ankle that was the last to regain all feeling some time the following day.
And just like that, hour by hour, me and my new hip made it into day 1 post op. I could not be more grateful for the care and good humour of all the staff at SWLEOC Epsom Hospital pre and post op that day. Friendly people, amazing professionals. Thank you all so much.
I made it through that first day. And now the post hip-revision journey begins.
More to follow in a few days…..thanks for reading the blog! Love to you all xx
Jill Pringle was born with bilateral hip dysplasia (DDH) in 1971. She writes this blog to share her experiences of walking and living with this common disability.